Definition and Causes:
DEFINITION:
What Is Coronavirus?
Coronaviruses (CoV) are a large family of viruses that cause a range of illnesses from a mild common cold to more severe diseases such as pneumonia (lung infection). These viruses can cause illness in humans and animals; rarely, animal coronaviruses can infect people, and these can then spread from person to person through close contact, for example, in a household, workplace, or health care facility (long term care facility/nursing home). The most recently discovered coronavirus causes Coronavirus disease (COVID-19).
Apart from COVID-19, the other coronaviruses that spread from animals to humans and can cause serious diseases are:
- Severe acute respiratory syndrome coronavirus (SARS-CoV)
- Middle East respiratory syndrome coronavirus (MERS-CoV)
Corona means crown. Coronaviruses are named for their appearance because of protein spikes on the surface of the virus resemble the sun’s corona.
What Is COVID-19?
The Coronavirus Disease 2019 or COVID-19 is an infectious disease caused by a new strain of the Coronavirus family, called SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2), that was first discovered in 2019 and was not previously identified in humans. This strain of Coronavirus was unknown until an outbreak of respiratory illness in Wuhan, China, led to the identification of the new coronavirus strain as the root cause of respiratory illness now known as Covid-19.
The COVID-19 is the name given by the World Health Organization (WHO) on February 11, 2020. In the name “COVID-19”, the “CO” stands for corona, the “VI” is for virus, and the “D” means disease. The “19” is for 2019, the year the disease first appeared in China.
CAUSES:
It’s unclear exactly how contagious the new coronavirus is. The virus can spread from person to person by respiratory droplets released when someone with the virus coughs or sneezes or exhales. An individual can catch the infection through:
- Close contact with an infectious person, typically within six feet of someone who is contagious
- Touching contaminated objects or surfaces (like doorknobs or tables or phones), then touching your eyes, nose, or mouth before washing your hands
- Breathing in droplets from an infected person who coughs or exhales droplets
Currently, health experts believe that COVID-19 cannot spread through the air over long distances or time and is mainly transmitted through contact with larger respiratory droplets. These droplets are too large and heavy to float in the air for longer distances and time, so they quickly land on objects and surfaces around the person who coughs or sneezes, making the area around the infected person contagious. These droplets typically spread only 1 to 2 meters; hence, current “social distancing” measures emphasize the importance of staying at least 2 meters away from others.
How long can the COVID-19 survive on surfaces?
It is not certain how long the COVID-19 virus survives on surfaces. It is generally assumed that it can survive from a few hours to several days depending on the type of surface, temperature, humidity of the environment, and some other factors. Current studies suggest COVID-19 survival with infectious capability is:
- In air: At least three hours
- On plastic and stainless steel: For at least 72 hours
- On cardboard: About 24 hours
- On copper: Less than 4 hours
Symptoms:
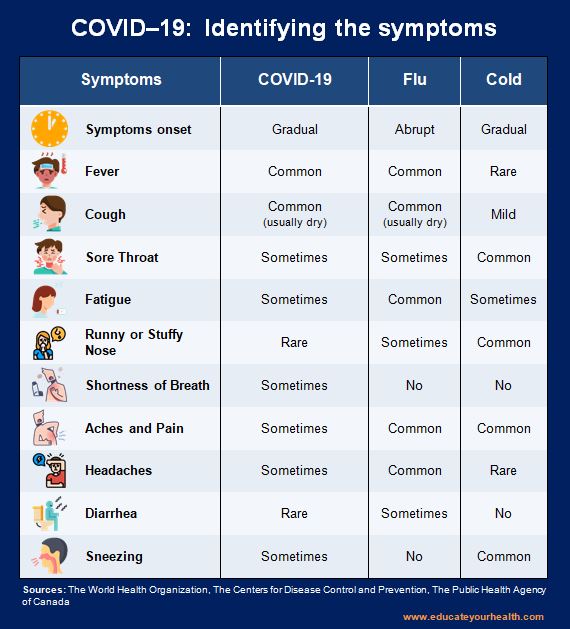
Individuals infected with COVID-19 may have little to no symptoms or symptoms that may be similar to other respiratory illnesses like flu and the common cold. Symptoms may appear 2 to 14 days after exposure to COVID-19, and in most cases, it appears approximately 4 to 5 days after exposure.
Most common symptoms include:
- Fever
- Cough (usually dry)
- Shortness of breath or difficulty breathing
- Sneezing
- Sore throat
- Extreme tiredness
- Decreased appetite
Less common symptoms are:
- Headache
- Stuffy or runny nose
- Productive cough
- Diarrhea
- Nausea / vomiting
- Unexplained loss of taste or smell reported by some patients
In children, symptoms can be:
- Diarrhea
- Runny nose
- Sore throat
- Lethargy
- Poor feeding
Generally, people recover from this disease without needing special treatment; however, sometimes it can progress to more serious illness and can cause pneumonia, bronchitis, kidney failure, and even death, especially in individuals with a high risk of serious illness such as the elderly or with pre-existing medical conditions like diabetes, heart disease, asthma or have weakened immune system.
If you have symptoms:
- Stay home
- Take the COVID-19 self-assessment
- Call your local Coronavirus (COVID-19) helpline or a health care provider for instructions and advice regarding testing
- Do not go to an Emergency (ER) unless you have a medical emergency
In case of a medical emergency:
- Call 911 or your local health emergency number
- Notify the operator of your emergency; if you also suspect that you may have COVID-19 or exposure to the virus explain this to the operator during your call
- If possible, put on a face mask before emergency medical services arrive
How to Differentiate COVID-19, Flu and Cold symptoms
Investigations and Treatment:
INVESTIGATION:
Coronavirus (COVID-19) infection is suspected based on symptoms and diagnosis is confirmed through laboratory tests. It is recommended and very important for everyone to self-isolate for 14 days after returning from travel outside of their country of residence and do self-assessments; if no symptoms are present then self-monitor for 14 days. If possible, assist those who require self-assessment and self-monitoring but are not able to do so by themselves.
Self-Assessment: (click to view and download)
If you are feeling unwell with any of the following symptoms:
- Fever, new cough or difficulty breathing (or a combination of these symptoms)
- Muscle ache, fatigue, headache, sore throat, runny nose, or diarrhea
- Symptoms in young children may also include lethargy, poor feeding, diarrhea, runny nose, and sore throat
AND you have any of the following:
- Have you travelled outside the country of residence in the last 14 days?
- Have you been in close contact with someone who has a confirmed or probable case of COVID-19 infection (e.g. someone in your household or workplace)
- Been in close contact with a person who is sick with respiratory symptoms (e.g. fever, cough, or difficulty breathing) who recently travelled outside the country of residence
If you answered yes to these questions, you should seek clinical assessment for COVID-19 over the phone and may need a laboratory test for the confirmation of diagnosis.
- Contact your local Coronavirus (COVID-19) helpline or a health care provider or Public Health Authority and let them know that you have used this self-assessment tool
If you answered no to these questions, it is unlikely that you have COVID-19.
You are recommended to:
- Continue self-monitoring of your health and may you need to go self-isolate for a full 14 days after your return to your resident country of residence or if you have had contact with someone who is ill. If you develop any new symptoms, seek clinical assessment and testing for COVID-19
Self-Monitoring: (click to view and download)
What and why you need self-monitoring?
You have no symptoms and
- There is a reason to believe that you have been exposed to a person with COVID-19
- You are in close contact with older adults or medically vulnerable people
- You have been advised to self-monitor for any other reason by your Public Health Authority
What to do in self-monitoring?
- Monitor yourself for 14 days for one or more signs and symptoms of COVID-19, such as:
- Fever (take and record temperature twice daily)
- Cough
- Runny nose
- Sore throat
- Difficulty breathing
- In children look for diarrhea, poor feeding, lethargy
- Continue your daily routine but avoid crowded places and increase your personal space from others, whenever possible
What to do if you develop these or any other symptoms?
- Self-isolate immediately and contact your local Coronavirus (COVID-19) helpline or a health care provider or Public Health Authority for instructions and testing
Self-Isolation: (click to view and download)
What and why you need self-isolation?
You have no symptoms and
- A history of possible exposure to the novel coronavirus due to travel outside of your country of residence
- You are in close contact with a person diagnosed with COVID-19
- Your Public Health Authority has identified you as a close contact of someone diagnosed with COVID-19
What to do in self-isolation?
- Stay at home and monitor yourself for symptoms of COVID-19, even if mild, for 14 days
- Avoid contact with other people to prevent the possible spread of the virus
- Obtain a supply of surgical masks (enough for 14 days)
- Frequent use of soap, water and/or alcohol-based hand sanitizer to clean your hands
- Watch for symptoms in yourself or a family member
- Stay in touch with family members and friends by telephone, email, or social media
- Ask someone to get food and other necessities for you and leave them at your front door
- If you have to visit your health care provider, avoid using public transportation such as subways, taxis, and shared rides. If unavoidable, wear a mask and sit in the back seat
What to do if you develop symptoms?
- If you develop symptoms, even if mild, within 14 days of returning from travel, or within 14 days of the last contact of a confirmed case, then isolate immediately, stay home, avoid other people, and contact your local Coronavirus (COVID-19) helpline or a health care provider or Public Health Authority immediately, you may need a laboratory test
Laboratory testing:
Currently is recommended for those individuals who meet the criteria for suspected cases, and specimen for laboratory testing can be collected either from 1 site or multiple sites, depending on the diagnostic criteria, and samples to be taken are saliva (sputum), a nasal swab and/or a throat swab.
Criteria for laboratory testing may be
You will be tested if your doctor decides you meet the criteria, such as:
- Returned from overseas in the past 14 days and you develop a respiratory illness with or without fever
- Have been in close contact with a confirmed COVID-19 case in the past 14 days and you develop a respiratory illness with or without fever
- Have severe community-acquired pneumonia and there is no clear cause
- A healthcare worker who works directly with patients and you have a respiratory illness and a fever
TREATMENT:
Most people with Coronavirus (COVID-19) illness have mild symptoms and recover on their own. Current management pf non-serious illness is directed towards isolation of patients to prevent the spread of the virus to others and supportive measures to relieve symptoms, such as:
- Use of pain relievers
- Cough syrup or other cough medication
- Rest
- Maintain fluid intake
- Humidifier or a hot shower might help with a sore throat or cough
- Supplemental oxygen in more severe cases
If your doctor thinks you can be treated at home, he or she may give you special instructions, such as to isolate yourself as much as possible from family while you’re sick and to stay home for a period of time. If you’re very ill, you may need to be treated in the hospital.
Note: Get medical attention immediately if you or any member of your family develop emergency warning signs for Coronavirus (COVID-19).
Emergency warning signs include but not limited to:
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest
- New confusion, drowsiness, or difficulty being aroused
- Bluish lips or face
MEDICATION:
There is a large-scale global effort to find various treatment options and develop vaccines for Coronavirus (COVID-19).
To-date, only one medication has been approved to treat COVID-19.
- Remdesivir: An antiviral drug, recommended for use in hospitalized adults and children who are age 12 and older and who require supplemental oxygen
The FDA has granted an emergency use authorization (EUA) for:
- Baricitinib
- Bamlanivimab
- Casirivimab and Imdevimab (combination)
An emergency use authorization (EUA) by the FDA is a temporary authorization and is not the same as drug approval, and is meant to provide access to medicine in an emergency.
VACCINES:
There are more than 145 COVID-19 vaccines researchers are testing, out of this about 58 clinical trials on humans and at least 87 preclinical vaccines are under active investigation in animals.
Large-scale clinical trials are in progress or being planned for five COVID-19 vaccines in the United States:
- Comirnaty (known as Pfizer/BioNTech COVID-19 vaccine): Claiming an efficacy rate near 95 percent. Need to store at ultra-low temperature. The vaccine triggers the body’s natural production of antibodies and stimulates immune cells to protect against COVID-19 disease and is authorized to in individuals 16 years of age or older
- Health Canada approved the vaccine to individuals 5 years of age or older
- The United Kingdom gave emergency authorization on December 2, 2020
- Unites States of America:The U.S. Food and Drug Administration (FDA) approved the vaccine on August 23, 2021, to individuals 16 years of age or older. Comirnaty is authorized for use in individuals 5 years and older. Everyone ages 12 years and older is recommended to get a booster shot
- European Union (EU): European Commission (EC) has granted a conditional marketing authorization (CMA) on December 21, 2020
Dosage:
It is a 2-dose schedule vaccine and the vaccine is given by injection [30 micrograms (0.3 ml )]) into the muscle of the arm and then a second dose 21 days later.
Vaccine effectiveness in preventing COVID-19 infection beginning 7 days after the second dose (this means that protection is achieved 28 days after the initiation of the vaccination)
Possible side effects:
Like common side effects as of other vaccines, Pfizer/BioNTech COVID-19 vaccine’s possible side effects included pain at the site of injection, redness or swelling at the injection site, body chills, feeling tired, and feeling feverish which generally goes away within a few days of appearing. It’s rare but as with all vaccines, there is a chance that there will be a serious side effect.
Note: Individuals who are hypersensitive to the active substance or to any ingredient in the formulation of Pfizer-BioNTech’s COVID-19 vaccine shouldn’t get it, and individuals with a history of significant allergic reactions to a vaccine, medicine, or food including a previous history of anaphylactoid reactions should consult their healthcare provider for the vaccine.
- Moderna COVID-19 vaccine: Claiming an efficacy rate of near 95 percent. Need to store at low temperature. The vaccine triggers the body’s natural production of antibodies and stimulates immune cells to protect against COVID-19 disease and is authorized in individuals 18 years of age or older
- Health Canada authorized the use of the vaccine in Canada in individuals 12 years of age or older
- Unites States of America: On January 31, 2022, The U.S. Food and Drug Administration (FDA) approved the vaccine in individuals 18 years of age and older
Dosage:
It is a 2-dose schedule vaccine and the vaccine is given by injection [100 micrograms (0.5 ml)] into the muscle of the arm and then a second dose 28 days later.
Vaccine effectiveness in preventing COVID-19 infection beginning 14 days after the second dose.
Possible side effects:
Like common side effects as of other vaccines, the Moderna COVID-19 vaccine’s possible side effects included pain at the site of injection, redness or swelling at the injection site, body chills, feeling tired, and feeling feverish which generally goes away within a few days of appearing. It’s rare but as with all vaccines, there is a chance that there will be a serious side effect.
Note: Individuals who are hypersensitive to the active substance or to any ingredient in the formulation of Moderna COVID-19 vaccine shouldn’t get it, and individuals with a history of significant allergic reactions to a vaccine, medicine, or food including a previous history of anaphylactoid reactions should consult their healthcare provider for the vaccine.
- Oxford-AstraZeneca COVID-19 vaccine: A Viral vector vaccine, claiming an effectiveness of about 62% in preventing symptomatic COVID-19 disease. Need to store at the standard fridge, 2°C to 8°C (36°F to 46°F). The viral vector used in the Oxford-AstraZeneca COVID 19 Vaccine is based on a naturally occurring, low-prevalence chimpanzee adenovirus. It stimulates the body’s natural defences (immune system), by causing the body to produce its own protection (antibodies) against the SARS-CoV-2 virus that causes the COVID-19 infection. In this form, the vaccine cannot cause COVID 19 or adenoviral disease. The vaccine and is authorized in individuals 18 years of age or older, and there is limited information from clinical trials on the efficacy of the Oxford-AstraZeneca COVID-19 Vaccine in individuals ≥65 years of age
- Health Canada with terms and conditions authorized the use of the vaccine in Canada on February 26, 20
- The European Commission: European Commission (EC) has granted a conditional marketing authorization (CMA) on January 29, 2021
- The United Kingdom gave emergency authorization on December 30, 2020
Dosage:
It is a 2-dose, schedule vaccine, and the vaccine is given by intramuscular injection (0.5 mL) and then a second dose be administered between 4 and 12 weeks after the first dose.
Possible side effects:
Like common side effects as of other vaccines, the Oxford-AstraZeneca COVID-19 vaccine’s possible side effects included pain at the site of injection, redness or swelling at the injection site, body chills, feeling tired, and feeling feverish which generally goes away within a few days of appearing. It’s rare but as with all vaccines, there is a chance that there will be a serious side effect.
Note: Individuals who are hypersensitive to the active substance or to any ingredient in the formulation of the Oxford-AstraZeneca COVID-19 vaccine shouldn’t get it, and individuals with a history of significant allergic reactions to a vaccine, medicine, or food including a previous history of anaphylactoid reactions should consult their healthcare provider for the vaccine.
- Janssen COVID-19 vaccine: Claiming an efficacy rate of near 67 percent against Covid-19, the vaccine was approximately 77% effective in preventing severe/critical COVID-19 occurring at least 14 days after vaccination and 85% effective in preventing severe/critical COVID-19 occurring at least 28 days after vaccination. Need to store at the standard fridge, 2°C to 8°C (36°F to 46°F). It is the viral vector vaccine, based on a naturally occurring, low-prevalence human adenovirus. The vaccine cannot cause COVID‑19 or adenoviral disease and is authorized in individuals 18 years of age or older
- Unites States of America: The U.S. Food and Drug Administration (FDA) issued Emergency Use Authorization (EUA) on February 27, 2021
- Health Canada with terms and conditions authorized the use of the vaccine in Canada on March 5, 2021
Dosage:
It is a single dose vaccine and the vaccine is given by injection (0.5-mL) into the muscle of the upper arm.
People had the most protection 2 weeks after getting vaccinated.
Possible side effects:
Like common side effects as of other vaccines, the Janssen COVID-19 vaccine’s possible side effects included pain at the site of injection, redness or swelling at the injection site, body chills, feeling tired, and feeling feverish which generally goes away within a few days of appearing. It’s rare but as with all vaccines, there is a chance that there will be a serious side effect.
Note: Individuals who are hypersensitive to the active substance or to any ingredient in the formulation of the Janssen COVID-19 vaccine shouldn’t get it, and individuals with a history of significant allergic reactions to a vaccine, medicine, or food including a previous history of anaphylactoid reactions should consult their healthcare provider for the vaccine.
- Novavax: Waiting for their safety and efficacy rate data
Isolation: (click to view and download)
What and why you need isolation?
You have
- Been diagnosed with Coronavirus (COVID-19)
- Symptoms, even if mild and are waiting to hear the results of a laboratory test for Coronavirus (COVID-19)
- Been advised to isolate at home for any other reason by your Public Health Authority
What to do in Isolation?
- Stay at home until your Public Health Authority advises you that you are no longer at risk of spreading the virus to others
- Avoid contact with other people to help prevent the spread of disease in your home and in your community, particularly to those at high risk of severe illness such as older adults or medically vulnerable people
- Keep in touch with family members and friends by telephone, email, or social media
- If possible, keep up normal daily routines; eat healthily, and exercise
What to do if symptoms get worse?
- Seek immediate medical attention. If 911 activated, explain your symptoms and reason of isolation to the operator
Coronavirus (COVID-19) and Mental health: (click to view and download)
This outbreak of Coronavirus (COVID-19) impacts everyone, disrupting lives, and routines around the world. It is very important during this time that while taking preventive measures, your mental health, and that of your friends and family, especially children and adolescents should not be forgotten. The COVID-19 outbreak has lead to stress, panic, fear, and increased anxiety which is understandably a natural reaction to this type of situation.
While anxiety is the natural response, functioning as an alert system that helps us stay vigilant and respond to potential dangers, it should not escalate to interfere with daily health and wellness. Mental health stress can affect us in many ways, and everyone reacts differently, such as:
- Fear and worry about your own health and of your loved ones
- Panic buying (e.g. toilet paper and canned goods)
- Difficulty concentrating or sleeping
- Changes in eating patterns
- Frustration, irritability, or anger
- Feeling helpless
- Increased use of alcohol, tobacco, or other drugs
How to cope with stress, anxiety or distress?
- Remind yourself that COVID-19 is a serious but temporary illness and that in time, life will return to normal
- Make time to consider how to take advantage of unexpected flexibility in your daily routine
- Create a schedule for yourself and your children
- Social isolation means physical distancing. Stay connected with your friends, family, and others by e.g. telephone, text, FaceTime, or video chatting
- Try to do some engage in other activities you enjoy
- Take breaks, hearing about the pandemic repeatedly can be upsetting
- Avoid rumors and fake news
- Stay connected to your official health news and recommendations for accurate information
- Take care of your body
- Eat healthy, well-balanced meals
- Exercise regularly (including stretching and deep breathing exercises)
- Get plenty of sleep
- Mindfulness meditation might help reduce stress
- Avoid increase use of alcohol or other drugs and smoking
Children and adolescents:
- Try not to pass your anxiety on to your children
- Reassure your children that they are safe with the measures being undertaken to control the pandemic
- Parents take time to talk to children about what’s happening, listen to their concerns, and answer their questions realistically
- Maintain regular routines and schedules as much as possible, or help create new ones in a new environment, including school/learning as well as time for safely playing and relaxing
- Encourage children to draw, write, or journal so they can express their feelings
- Parents teach good hand-washing practices and let the children know that all the adults in their lives are working hard to keep them safe
- Give them extra love and attention
Be Prepared:
COVID-19 is a pandemic. The virus is actively spreading everywhere around the globe and affecting almost every sector of life and business. Prepare for this pandemic. Familiarize yourself with self-assessment, self-monitoring tools. Be prepared for possible self- or mandated isolation within your home for up to 14 days; ensure that you or an affected family member have enough supplies to avoid leaving your home in the event that you have to isolate or become ill. Being prepared for this outbreak can help protect your health and the health of those you care about in the event of an outbreak of COVID-19 in your community.
- How to prepare yourself for Coronavirus (COVID-19) pandemic? (click to view and download)
Risk Factors and Prevention:
RISK FACTORS:
Risk factors for COVID-19 appear to include:
- Recent travel from or residence in an area with the ongoing spread of COVID-19 as determined by Health Canada or Centers for Disease Control and Prevention (CDC) or the World Health Organization (WHO)
- Close contact with someone who has a confirmed or probable case of COVID-19 infection
- Elderly persons (those greater than 65 years old)
- Compromised immune system due to:
- Chemotherapy or radiation therapy
- Organ or bone marrow transplant
- Use of high doses of corticosteroids
- HIV or AIDS infection
- Persons who have serious chronic medical conditions including:
- Heart disease
- Diabetes
- Lung disease e.g. asthma
PREVENTION:
Take common sense precautions to help prevent the spread of all infectious diseases, including COVID-19. The best way to prevent illness is to avoid being exposed to the virus and follow the accurate public health advice from the WHO and your local health authorities.
- Avoid close contact with people who are ill, if possible
- Wash your hands frequently with soap and water for at least 20 seconds at a time especially after you have been in a public place, or after blowing your nose, coughing, or sneezing
- Use alcohol-based hand sanitizer containing at least 60 percent alcohol if soap and water are not available. Cover all surfaces of your hands and rub them together until they feel dry
- Avoid touching your eyes, nose, and mouth with unwashed hands
- Cover your mouth and nose with a tissue, or use the inside of your elbow, when you cough or sneeze
- Do not reuse tissue after coughing, sneezing, or blowing your nose, throw used tissues in a lined wastebasket and wash your hands afterward
- As much as possible keep at least 1-2 meters distance between yourself and others
- Clean and disinfect surfaces that are frequently touched
- Avoid all non-essential travel
- Social distancing (physical)
- Staying at home
- Avoiding large public gatherings if they’re not essential
- Minimize physical contact, especially with people at higher risk, such as the elderly and people with existing health conditions
- Avoid sharing food, dishes, glasses, bedding, and other household items if you’re sick
Steps to protect others:
- Stay home if you’re sick
- Wear a facemask if you are sick when you are around others (e.g. sharing a room or vehicle) and before you enter a healthcare provider’s office
- If for any valid reason you are not able to wear a facemask (e.g. trouble breathing), then do your best to cover your coughs and sneezes
- Clean and disinfect frequently touched surfaces daily e.g. tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks
- If surfaces are dirty, clean them: Use detergent or soap and water prior to disinfection
- Follow the self-isolation criteria
- Avoid having visitors to your home
- If possible, have supplies delivered to your home instead of running errands
Outcome:
The COVID-19 outbreak has had a significant impact on society, not only from the health/healthcare perspective but there has also been a tremendous impact on socialization, and the economy, the latter creating a global economic and labour crisis.
Fortunately, most people infected with coronavirus illness will have mild cold/flu symptoms and will recover on their own. However, every infected person is at risk of an acute change in symptoms with the development of more severe respiratory illness. Current information suggests that the elderly and with chronic health conditions, particularly those with the weakened immune system, are at higher risk of developing more severe illness or complications such as:
- Pneumonia
- Bronchitis
- Organ failure such as kidney failure
- Irregular heart rate / heart damage
- Some neurological complications also reported
- Death
Coronavirus (COVID-19): Myth vs. Fact
MYTH: 5G mobile networks spread COVID-19.
5G radiation does not allow viruses to penetrate the skin and there is no evidence 5G radio frequencies cause or exacerbate the spread of the coronavirus (COVID-19).
MYTH: The new coronavirus (COVID-19) was deliberately created in a laboratory and released into the environment.
Officials believe the new coronavirus outbreak occurred when a virus that commonly occurs in an animal, such as a pig, bird or bat, underwent natural changes that allowed it to transfer to humans.
MYTH: The new coronavirus (COVID-19) is a bioweapon.
There isn’t any evidence of anything other than a naturally occurring virus.
MYTH: The new coronavirus (COVID-19) may not survive in areas with extreme climates e.g. hot and humid climates.
The WHO advises that there’s no reason to believe that the weather will impact the new coronavirus. Since the normal human body temperature remains around 36.5°C to 37°C, regardless of the external temperature or weather, the virus can be shared among persons in close contact.
MYTH: It is necessary to always wear a homemade mask when leaving home.
It is not necessary to wear homemade masks continually after you leave your home, as the masks could become soiled or contaminated with other bacteria and viruses, which will make the mask unsanitary. It is not necessary to wear a mask when walking in open spaces, or traveling in a car by yourself, or with other members of your household. Masks, however, may be most helpful in confined areas (such as grocery stores) particularly if social distancing is a concern.
MYTH: Home remedies can cure and protect against COVID-19
No home remedies have been proven can protect against COVID-19, including essential oils, silver colloid, sesame oil, garlic, fish tank cleaner, burning sage, and sipping water every 15 minutes.
MYTH: The COVID-19 virus can be transmitted by mosquitos.
At this time, there is no data to suggest that COVID-19 or other similar coronaviruses (e.g. SARS, MERS) are spread by mosquitoes or other parasites.
MYTH: Taking Vitamin C, Vitamin D, or any other supplement will prevent COVID-19.
There is no evidence to support that taking any supplement will prevent COVID-19 infections.
MYTH: Young people are not susceptible.
People of all ages can be infected by the coronavirus (COVID-19). Older people and those with pre-existing medical conditions, such as asthma, diabetes, and heart disease, appear to be more vulnerable to severe illness that can be caused by the new coronavirus.
MYTH: You can avoid the COVID-19 virus by drinking warm water every 15 minutes.
There is no evidence at all to support this claim.
MYTH: Hand dryers are effective in killing the COVID-19 virus.
No, the heat from hand dryers is not effective in killing COVID-19.
MYTH: Spraying alcohol or chlorine all over your body kills the COVID-19 virus.
No. Spraying alcohol or chlorine on your body will not kill COVID-19. In fact, spraying such substances can be harmful to delicate mucous membranes including your eyes, nose, and mouth.
MYTH: Some antibiotics are effective in preventing and treating the COVID-19 virus.
No. Antibiotics do not work against viruses, such as COVID-19, they only work against bacteria.
MYTH: There are specific medicines to prevent or treat the COVID-19 virus.
To date, there is no specific medicine recommended to prevent or treat the virus that causes COVID-19.
MYTH: Can taking a hot bath prevent from COVID-19?
Taking a hot bath will not prevent you from catching COVID-19. Regardless of the temperature of your bath or shower, your normal body temperature remains at around 36.5°C to 37°C.
Myth: There is a vaccine available to cure COVID-19.
No. Unfortunately, there is no vaccine for the Coronavirus (COVID-19) at present, but research scientists have already begun working towards the development of a vaccine. However, it will take some time to develop a vaccine that is safe and effective in human beings.
MYTH: Can regularly rinsing your nose with saline help prevent infection with the COVID-19 virus?
No. While there is some limited evidence that regularly rinsing nose with saline can help people recover more quickly from the common cold, there is no evidence that regularly rinsing the nose with saline protects people from infection with the new coronavirus.
MYTH: Eating garlic help prevent infection with the COVID-19 virus.
No. The WHO advises that there is no evidence from the current COVID-19 outbreak to suggest that eating garlic will protect people from the virus.
MYTH: Receiving a letter or package from China will make a person sick.
No. Currently, from the available research data, people receiving packages from China are not at risk of contracting the new coronavirus. Based on previous analysis, the WHO reported that the coronavirus does not survive on letters and packages for an extended time.
For anyone concerned that a surface has been contaminated, the health agency advises cleaning it with a disinfectant. If someone has already touched it before it’s been cleaned, they should immediately wash their hands with an alcohol-based hand rub or with soap and water.
Myth: Thermal scanners can diagnose people infected with the COVID-19 virus.
No. Thermal scanners can detect people who are sick with a fever from any cause, such as seasonal flu, and not specific for those infected with COVID-19.