Definition and Causes:
Acute myocardial infarction (MI or heart attack) occurs when there is lack of oxygen to the heart muscle (ischemia), resulting from the interrupted blood supply, and leading to tissue damage or cell death (infarction); usually due to blockage within the blood vessels supplying the heart (the coronary arteries).
CAUSES:
- Atherosclerosis (hardening of blood vessel and narrowing of the lumen of the arteries), due to the formation of plaque on the walls of the vessels. Plaques are in part caused by a collection of cholesterol/lipids and white cells. Plaque rupture leads to blood clot formation on top of the plaque and blockage of the blood vessel
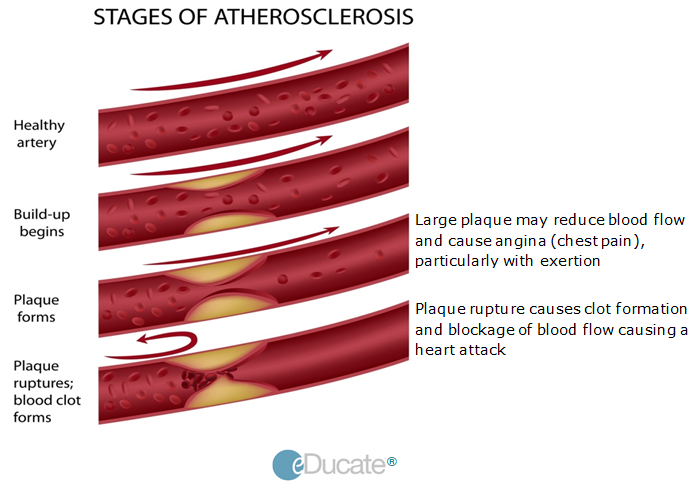
Atherosclerosis: Risk factors including aging, high blood pressure, high cholesterol, smoking, and diabetes leads to hardening (and narrowing) of the coronary arteries as well as plaque formation. Plaque rupture underlies clot formation and vessel occlusion.
- Dissection or tearing of the large artery (the aorta) that carries blood away from the heart to the body. During the dissection, a tear occurs within the inner lining of the artery. If a dissection occurs within the aorta close to the heart, the blood supply to the heart through the coronary arteries may be reduced and in some cases may a cause a heart attack
- Some medications or illicit drug (e.g. cocaine) can lead to undue narrowing or spasms within the coronary vessels, reducing blood flow and causing a heart attack
Symptoms:
Chest Pain (angina)
- Chest pain or discomfort for >20 minutes
- Moderate to severe in intensity
- Persistent and continuous
- Pain may feel heavy, squeezing, crushing, stabbing or burning
- May radiate to:
- Arms
- Abdomen
- Back
- Lower jaw
- Neck
- 25% of individuals with ischemia (decreased blood flow from coronary vessels to the heart muscle) do not experience chest pain

Other associated symptoms:
- Lightheadedness/dizziness
- Excessive sweating
- Fatigue/restlessness
- Syncope (loss of consciousness and/or posture)
- Shortness of breath on lying down
- Nausea/vomiting
- Cold clammy skin
- Rapid or irregular pulse
Investigations and Treatment:
Patients presenting with angina (chest pain) or suspected of suffering from a heart attack will undergo a number of diagnostic examinations. Doctors will inquire about the patient’s present and past medical history, family history of heart or other vascular diseases (e.g. stroke) as well as perform a physical examination, blood work, ECG and may use a number of additional diagnostic tests.
History:
- Location of chest pain / associated symptoms (jaw pain, sweating, etc.)
- Duration: Does the chest pain last for more than 20 minutes?
- Past history of heart attack or angina
- Previous cardiac surgery or coronary intervention (balloon angioplasty)
- History of syncope (fainting) after pain onset
- Presence of risk factors (e.g. high blood pressure, smoking, etc.)
Physical Exam:
Chest
- Pain/tenderness
- Heart and lung sounds (stethoscope)
- Respiratory (breathing) rate
Pulse rate and blood pressure:
- Increased or decreased
Extremities (toes, fingers)
- Cool temperature
- Loss of color
- Swelling (edema)
Neck:
- Pain radiation (jaw, back, arm)
Abdomen:
- Pain/tenderness
Laboratory Tests:
- Blood work for cardiac biomarkers (special proteins that might indicate heart muscle injury e.g. troponin)
- Routine blood work and urine samples (as requested by treating physician)
Imaging:
- During an ECG, small patches with wire connections are attached to the skin across the chest and on an arm or leg. These detect the small electrical signals from the beating heart muscle which can be displayed on a screen, or printed, allowing the physician to examine the patient’s heart rhythms
ECHO (Echocardiogram):
An ultrasound of the heart which shows the heart valves and chambers (atria and ventricles) as well as blood flow
- Trans-Thoracic ECHO (TTE): Conducted across the chest wall. With the patient lying on an examining table a small amount of gel is placed on the left chest and a probe is used to generate sound waves into the chest cavity that produces a video image of the heart
- Trans-Esophageal ECHO (TEE): Conducted through the mouth. Patients may be mildly sedated and throat numbed (anesthetized). A narrow tube with a small probe is passed down the throat into the esophagus and an ultrasound image of the heart obtained
Chest X-ray:
- Used to visualize the lungs and heart to look for heart enlargement or fluid in the lungs
- A small tube (catheter) is placed into a blood vessel (usually in the groin area) and advanced through the vessels towards the heart. A dye is then injected into the blood vessels close to the heart. This technique allows doctors to see an image of the coronary arteries and so provides information regarding blocked vessels
- The extent and location of blockages are used to determine treatment, which might be medication only or bypass surgery or balloon angioplasty and stenting

Treatment:
Balloon angioplasty and stenting of the coronary vessel is the treatment of choice for most acute heart attacks. However, in some cases, medical management alone might be sufficient, while in others with severe blockages bypass surgery might be used.
Medications:
Some agents that may be used during a heart attack include:
- Antiplatelet drugs (e.g. aspirin)
- Helps to reduce blood clotting, and thus aiding blood flow to the heart
- Blood vessel dilator (e.g nitroglycerin):
- Temporarily opens arterial blood vessels during angina, improving blood flow to the heart muscle
- Pain relievers (analgesics e.g morphine):
- Helps to relieve chest pain
- Clot-busting drugs (e.g. tissue plasminogen activator; tPA, TNK-tPA):
- Not as effective as balloon angioplasty. May be considered when angioplasty and stenting are not available. These thrombolytic (clot-busting) agents are administered during a heart attack to dissolve the clot, allowing blood to flow to the heart muscle thereby minimizing damage
Some agents that may be used following a heart attack to prevent recurrence or other complications (e.g. stroke) include:
- Blood pressure (BP) medications:
- Controls (BP), reduces atherosclerosis (“hardening” of the blood vessels) and recurrence. Some BP medications also control heart rate ( e.g. beta blockers)
- Cholesterol-lowering medications (e.g. statin agents):
- May also be helpful in improving survival if given soon after a heart attack. Long term use may prevent a recurrence
- Blood-thinning medications (anticoagulants):
- May be used in some patients during an acute heart attack and also be used long term in select patients to prevent vascular complications e.g stroke
Some commonly used drugs in the treatment of heart attack are shown below:

Cholesterol-lowering medications:

Blood pressure medications with some common trade names are shown below:

Risk Factors and Prevention:
Non-modifiable risk factors:
- Age
- Congenital heart disease (heart conditions that a person may be born with)
- History of prior heart attack or stroke
- Family history of heart disease
Modifiable risk factors:
- High blood pressure
- High blood cholesterol
- Smoking
- Diabetes mellitus
- Obesity
- Sedentary lifestyle
- Alcohol and drug abuse (e.g. cocaine)
Outcome:
- Early recognition of symptoms and treatment can minimize heart muscle damage and prevent death
- 30% of patients with irregular chest pain have a heart attack within 3 months of the onset of the pain
- Heart attack patients should follow guidelines on lifestyle and behavior management as indicated by a doctor or other qualified health care professional to minimize recurrence